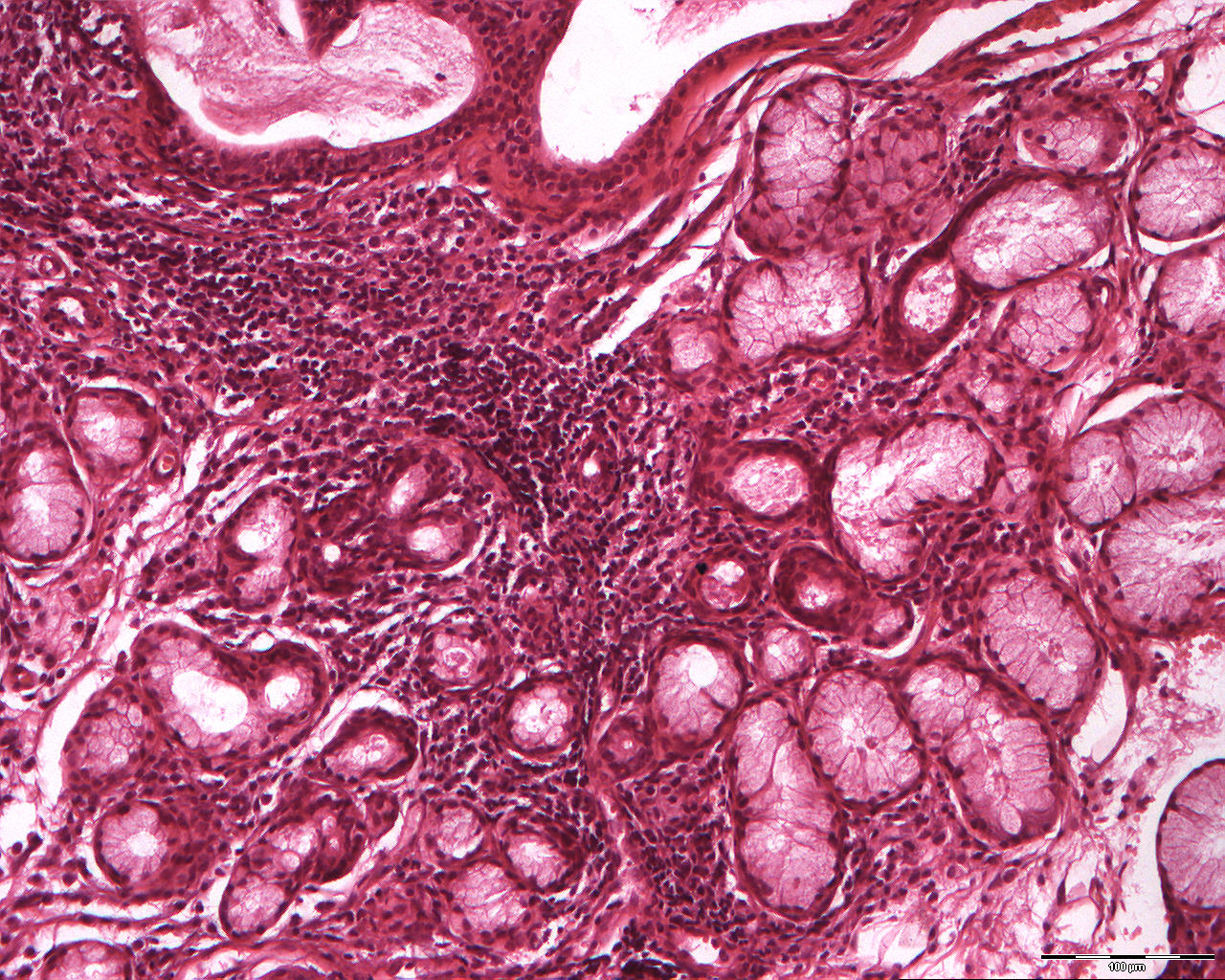
Intense chronic sialadenitis compatible with manifestation of Sjögren's syndrome (200X)
Clinical information: A 61-year-old woman presented herself with a dry oral mucosa (xerostomia) and a painful, red, fissured dorsum of the tongue with atrophy of the papillae. The patient had rheumatoid arthritis and was treated with prednisolone and acetylsalicylic acid.
Clinical diagnosis: Sjögren's syndrome?
Biopsy: 6 small labial salivary glands were removed.
Microscopic examination: Small seromucous salivary glands with focally pronounced parenchymal loss and dilated, irregular, mucus-filled, intralobular ducts are seen. Flattened epithelial lining in some places (epithelial atrophy) is seen. Mild to moderate lymphoplasmacytic infiltration and numerous large infiltrates of lymphocytes and plasma cells are also seen. There is also moderate stromal fat infiltration.
Comment: The histological picture in small labial salivary glands in Sjögren's syndrome is not pathognomonic and only shows a chronic sialadenitis. According to current criteria (2005), the presence of at least one mononuclear infiltrate (over 50 cells/4 m2 of tissue) is compatible with the manifestation of Sjögren's syndrome. The changes in the small labial salivary glands are often very localised, and it is essential that an adequate number (4-7) of the glands be examined. The diagnosis of Sjögren's syndrome is made on the basis of a number of criteria, among which a positive lip biopsy will be able to support the diagnosis but is not necessary.